Onondaga County sees rise in substance abuse, mental health crises
Onondaga County sees rise in substance abuse, mental health crises
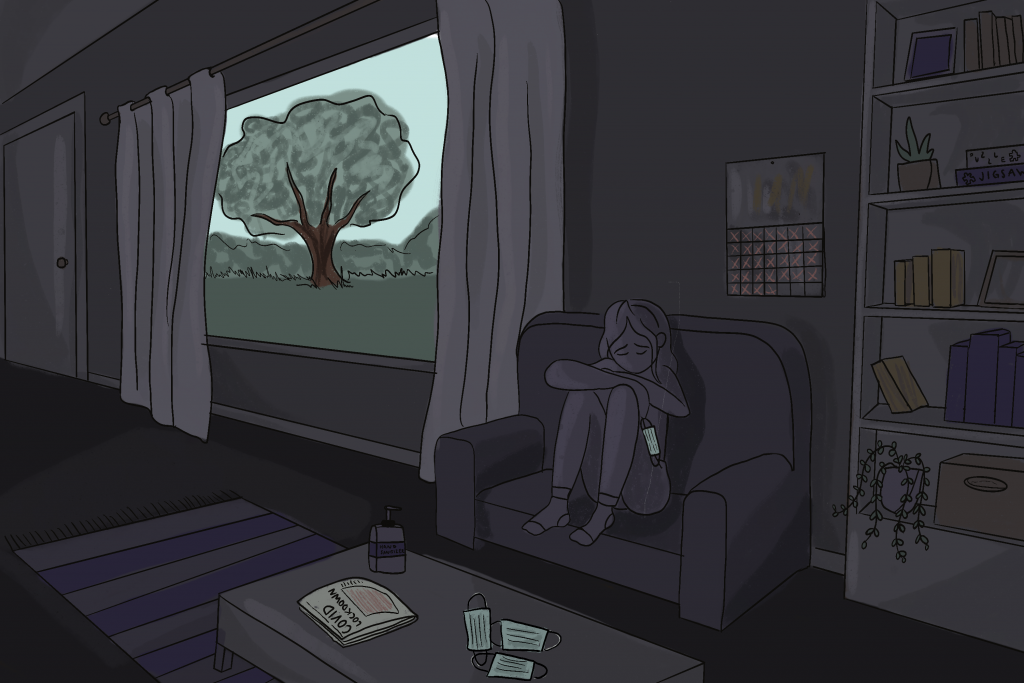
Substance abuse, overdoses, and calls for mental health support are all up in the first six months of 2020 as the pandemic takes a mental toll on Onondaga County, community health experts say.
According to the Onondaga County Opioid Epidemic Data Report, there were 41 unintended opioid-related deaths in Onondaga County in the first quarter of 2020 — this is more than double the 19 reported deaths seen in the same quarter of 2019.
The data through the second quarter, although not publicly released yet, shows an increase in unintended opioid-related deaths over the last year and several years before, said Mariah Senecal-Reilly, program coordinator at Onondaga County Health Department.
There has also been an increase in people seeking mental health help, such as making calls to local crisis hotlines. Kristine Knutson, the program coordinator of Crisis Intervention Services at Contact Community Services, said both their 211 hotline and the National Suicide Prevention Lifeline has had an increase in activity.
“It’s certainly a cause for real concern,” said Afton Kapuscinski, director of the Psychological Services Center at Syracuse University. “While we’re trying to prevent the spread of [COVID-19], and help with preventing death and trauma in that sense, we also want to balance that by looking at how we can better improve access and availability of mental health care to prevent other ways that people may be coming at risk for death and trauma.”
Some individuals in the Syracuse community who were already seeking treatment are reporting more symptoms of depression, anxiety, and alcohol or drug use, Kapuscinski said.
Onondaga County only seems to be reflecting national trends of a pandemic-related mental health crisis. The CDC reported in late June that 40% of U.S. adults reported struggling with mental health or substance abuse, 13% of which started or increased substance use.
This rise in mental health issues and substance use may be attributed to social isolation, which is a major risk factor for depression; dangerous home environments; fear of getting sick or dying; and financial stressors, Kapuscinski said.
This drug crisis presents an even more deadly threat because of the changes in drug supply as a result of the pandemic, said Alessandra Miller, director of Drug User Health at ACR Health. Many people no longer have reliable dealers, and are instead turning to people who are selling unknown products that are often laced with fentanyl which has led to more overdoses, Miller said.
Many programs have gone underfunded and understaffed when the community seems to need them most due to financial strains caused by the pandemic.
ACR Health had to furlough 70 of their staff members due to a lack of funding through the state, said Miller. When programs like ACR, which engage in life-saving services such as syringe exchange, Narcan, and medication-assisted treatment, are limited in their service they are unable to provide resources and services to people in need, said Miller.
The lack of these resources increases the likelihood of contracting communicable diseases and physical health issues as a result of substance use because of the inability to get a clean needle or receive treatment.
Following this spike in the first 3 months, U.S. Rep. John Katko introduced the Coronavirus Mental Health and Addiction Assistance Act: bipartisan legislation to create emergency grants for counties and Central New York community-based organizations that help those dealing with substance use.
However, places like ACR are not eligible for these funds because they are not a licensed NYS Office of Addiction Services and Supports (OASAS) facility, said Miller.
ACR solely relies on Department of Health funding, however, because New York state was hit hard financially as a result of COVID-19 they continue to be underfunded, said Miller.
Some programs, like hotlines, are trying to make up for the increased need through volunteers. Kapuscinski said she received emails from local and state hotlines looking to recruit psychologists and other mental health providers such as herself.
Many resources are trying to adapt their services to be remote.
Senecal-Reilly, program coordinator at Onondaga County Health Department, said one of the most important things the Onondaga County Health Department is working to do is make naloxone and Narcan, medications that treat overdoses, as widely available as possible. The department is working on implementing online naloxone training, which would provide people with a low-barrier way to access free naloxone, as opposed to having to go to in-person training or to the pharmacy, she said.
Similarly at ACR, patients can now speak with a nurse practitioner by phone or video chat to receive the prescriptions for their medication. As a result, they have seen an increase in attendance of scheduled appointments, said Miller.
The most important change that can be made to help combat the prevalence of substance use is dismantling the stigmas that exist around substance use, said Senecal-Reilly.
“People feel a lot of shame when they are struggling with substance use disorder,” said Senecal-Reilly. “If we can lessen the stigma, that would help the most in getting people into the services and treatment that can help them stay safe.”
Knutson said it is as simple as spreading the word about the resources that exist and extending kindness to those who might be struggling with their mental health.





